Research teams at IISc have been focusing on low-cost, scalable engineering solutions to back up a stressed healthcare system
Early on during the global spread of COVID-19, from the experiences of countries like Spain and Italy, it was clear that healthcare systems would be under pressure. Severe symptoms in COVID-19 patients include difficulty in breathing, typically requiring stays in Intensive Care Units (ICUs). Given the sheer number of people requiring breathing assistance and intensive care, a strain on resources was anticipated. “The pandemic is a logistical nightmare, not a medical nightmare,” says Dr Justin Gopaldas, Senior Consultant at the Intensive Care Unit and expert in critical care, Manipal North, Bangalore. “Managing the patients is rarely a problem in COVID-19 cases – managing the number of patients is,” he adds.
To deal with these unprecedented challenges effectively, it appeared that what was needed immediately wasn’t just brand new inventions, but also cost management in existing solutions and an ability to mass produce them if required, on a very short timeline. And as the closing of national borders was expected to severely affect international supply chains, these answers would have to be found locally. With these requirements in mind, a few teams at IISc have stepped up to examine how respiratory distress can be alleviated in ICUs using engineering solutions.
Low-cost ventilators
Modern mechanical ventilation, or assisted breathing, has historical references in medical literature dating back five centuries. In the 16th century, Flemish physician Andreas Vesalius described “blowing air into the lungs of an animal by inserting a tube into its trachea.” Ventilators in the early 1900s worked on ‘negative pressure ventilation’ mechanisms, where the atmospheric pressure around the body of a patient who cannot breathe is lowered. This reduced the pressure on the patient’s lungs, thereby creating a flow of air into the lungs. Modern-day ‘positive pressure ventilation systems’ apply pressure onto the patient’s respiratory system, forcing air into the lungs.
Some research groups at the Centre for Nano Science and Engineering (CeNSE) use Chemical Vapour Deposition (CVD) systems in which gases are mixed at varying pressures in a controlled way, and are then withdrawn from the system. The researchers quickly identified that this was, at the most basic level, the same principle used in a ventilator. Using this knowhow, and with some re-engineering to suit the need of the hour, they quickly got to work to develop ventilation solutions. After consulting with Dr Gopaldas, the team realised that under the circumstances, it would be more prudent to design and build a cheaper ventilation system using expertise and technology already at their disposal, than try to build ‘full-fledged ventilators’ (ventilators that can automatically sense when a patient needs air and can adjust the pressure and volume of air delivered as required).
The team realised that under the circumstances, it would be more prudent to design and build a cheaper ventilation system using expertise and technology already at their disposal
The team went on to develop different versions of the ventilator, which they call D0, D1, D2 and D3. Each version is more complex and offers more control than the previous one – while D0 uses the most basic zero-electronics ventilation, D1 uses solenoid-based pneumatics and electronics to cycle pressure-controlled air into the lungs. D2 allows almost all ventilation modes involving a continuous supply of air-oxygen mixture (Continuous Positive Airway Pressure or CPAP): mandatory and intermittent pressure and volume controlled ventilation; pressure regulated volume control (PRVC), inhalation and exhalation triggers, and about 30 alarm conditions. In addition to solenoids, it uses a proportional valve for better control. As of June 2020, D2 has completed 96 hours of continuous operation without failure. D3, their latest version, is an improved version of D2 that uses two proportional valves instead of one, offering more control to clinicians.
The team worked to make low-cost solutions, keeping in mind that in the case of ventilators, low cost doesn’t always mean the best option. Srinivasan Raghavan, Professor at CeNSE, says, “As an engineer, it’s very easy to get carried away and say, I want to make a cheap ventilator. But when you hear about the medical side, and you understand its challenges and how extremely complicated the human body is, you take a step back and sober up. Safety comes first. And only if that safety bar is overcome, should we think about cost.” Faculty and students from IISc and members of industry collaborated on this project, coordinated by Raghavan, in consultation with Dr Gopaldas at different stages.
Ventilators with local components
As the COVID-19 crisis unfolded and ventilators became a hot topic of discussion, it was a WhatsApp conversation on his college alumni group that first alerted Gaurab Banerjee, Associate Professor in the Electrical Communication Engineering Department, to the possibility that the pandemic’s spread would disrupt international supply chains. As a result, the availability of materials needed for healthcare solutions would be affected too. He and his friend Manas Pradhan, a Bangalore-based engineer and entrepreneur, quickly put a team together that would help design the ventilator, source the necessary equipment from the industrial supply chains within India and build the model of the instrument. That was the start of “Project Praana”, whose goal was to develop a full-fledged ICU-grade ventilator that uses locally sourced components. TV Prabhakar and HS Jamadagni – Principal Research Scientist and retired Professor respectively, in the Department of Electronic Systems Engineering (DESE), and Duvvuri Subrahmanyam and Pratikash Panda – both Assistant Professors in the Department of Aerospace Engineering, were also founding members of the team. The team also reached out to doctors and biomedical engineers on social media and received an overwhelming response from people across the country who were willing to help.
They identified two main industries that use technology potentially useful in building a ventilator: the water filter industry and the automobile industry. The pneumatics of a water filter that uses Reverse Osmosis hardware – which is used in several Indian households – could be adapted for a pressurised air-flow system. The food-grade containers in the water filter and the internal tubing could be used to mix gases required before delivering them to the patient. “It’s better to start with something that’s already food grade, since you may only have to make minor tweaks to adapt it for medical use,” says Banerjee. The team sourced pressure sensors needed in the ventilators from the automobile industry; several cars have pressure sensors that indicate when tyres are sufficiently inflated. These sensors can be used to regulate how much air needs to be pumped into a patient’s respiratory system.
Project Praana launched the first complete prototype of their ventilator model at the end of May 2020
Although the team wasn’t aiming to build a low-cost ventilator, the estimated cost of their product is Rs 1-1.5 lakh, which is substantially lower than other ventilators in the market at the moment (a basic commercial ventilator in the Indian market can cost about Rs 10 lakh and imported models can cost between Rs 25-30 lakh). Team Project Praana launched the first complete prototype of their ventilator model at the end of May 2020. Duvvuri Subrahmanyam, Assistant Professor in the Department of Aerospace Engineering, will lead the project at the manufacturing stage.
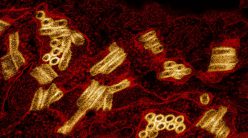
While the focus of Project Praana and the Sub-50,000 INR ventilator team has been to find a way to make new kinds of ventilators, the focus of one team in trying to meet the demand for ventilators, has been to create split valves (hotly discussed worldwide) so that existing ventilators can be shared by patients in an ICU. Akshay Naik, Associate Professor at CeNSE, and his team of students have fabricated and tested a design of 3D-printed valves for split use of ventilators in a hospital setting. In practice, shared use of ventilators is difficult, as no two patients may have exactly the same requirements, and while two patients may be able to use the ventilator with a splitter, there’s also the risk that both will receive a lower quality of treatment as a result. If needed in a crisis, the team at IISc has a tested and well-functioning design for these valves.
Another team is also working on a design for a “cyclone separator”, which can help extend the life of filters in ventilators and reduce the need for frequent maintenance. It is designed to remove oil droplets and dust particles in the air before it enters the ventilator. The compressor air is given a spin in a purpose-designed separation chamber. This causes the suspended matter to move outwards towards the wall where it adheres and does not re-enter the air flow. The clean air in the core is extracted by means of a central tube and is ready for final filtration before use.
Providing oxygen
Ventilators have been key in treating severe cases of COVID-19. But not all patients may need a ventilator; in many cases, patients may only require oxygen at a higher concentration. This treatment can be effective, life-saving, and cheaper than using a ventilator. A team led by Praveen Ramamurthy, Professor in the Department of Materials Engineering, has developed an “oxygen concentrator”, a device that separates out oxygen from the air around us to create a concentrated form of oxygen. This device can be deployed in healthcare systems in urban and rural settings where supply of oxygen for medical care may be challenging. It only requires a reliable power source and minimal maintenance.
Currently, oxygen concentrators are not manufactured in India. The team – Ramamurthy, Bhaskar K, retired Principal Research Scientist in the Electrical Engineering Department, and Arun D Rao, a former PhD student at the Department of Materials Engineering who now runs a startup, Reveron Pvt Ltd – built everything from scratch, including the hardware and software required for the device. They were able to achieve more than 92 percent concentration of oxygen with a flow rate from 1 litre per minute (lpm) to 10 lpm. Locally available components such as cartridges from the water filter supply chain, in-house designed electronics and housing were used to reduce costs. If necessary, these devices can also be integrated with ventilators.
A team led by S Dasappa, Professor at the Centre for Sustainable Technologies, has also been working on an “oxygen generator”. This team has used gas separation technology called vacuum swing adsorption to separate oxygen from the air. Ambient air is passed through an air-filter and then compressed and dried. Following this, it goes through a series of filters to remove impurities and contaminants. Finally, the gas is passed through a separation bed, where nitrogen is separated from oxygen, generating medical-grade oxygen. As it uses regular air as the input, the generator reduces dependence on oxygen cylinders and is particularly useful in semi-urban and rural areas. The equipment is suitable for small-scale medical facilities.
For those at IISc, focusing on solutions to manage the COVID-19 healthcare crisis has meant halting their existing research and working through strange and challenging new conditions like the lockdown. With restrictions on travel and interaction during the lockdown, some teams relied on help from IISc’s administration and the state government in order to get permission to travel to the suburbs to procure components for their devices. Much of their work has also been the result of collaboration with members of the research community, local businesspersons, fabricators, and industrial partners. Dr Gopaldas, who has interacted with many teams at IISc working on engineering solutions to COVID-19, says that the enthusiasm that drives them is infectious. “Although there has been a lot of constructive conversation on the healthcare front, the tone is one of impending doom. But during my visits to the research teams, I felt the energy!” That is something he has been able to bring back with him and translate to his own team at the hospital, he says.
Many teams have poured their hearts into developing low-cost, scalable solutions to help our already overworked healthcare system cope better with the pandemic. Raghavan hopes that, in spite of the hard work and time that he and his colleagues across the Institute have put into these innovations, they will not be needed. And the irony of the statement is not lost on him.
Priti Bangal is a Research Associate at IISc’s Centre for Ecological Sciences, and a science writing intern at the Office of Communications.
For more stories about the COVID-19 crisis, click on the links below:
Tracking the Scourge: Diagnostics, Testing and Vaccines for COVID-19
The Pandemic and Mental Health at IISc
Understanding COVID-19 Through the Lens of the Social Sciences