Why traditional antivenom therapy is inadequate in treating this neglected tropical disease

Humans have always been fascinated by snakes. In some cultures, snakes are considered divine because they are indispensable to humans in controlling rodent pests that can otherwise cause enormous damage to food crops. But snakes can also be deadly to humans, and have come to symbolise evil in mythology and popular culture. For instance, in the Book of Genesis in the Old Testament and the Torah, Satan takes the form of a serpent and talks Eve into eating the forbidden fruit from the tree of knowledge in the Garden of Eden.
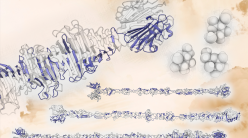
Several species of snakes are venomous (venomous animals actively inject toxins into their victims as opposed to those that are considered poisonous, which only harm animals that bite or eat them), and are capable of causing harm to humans through a process called envenomation. Snake venom is a toxic cocktail of proteins produced in modified salivary glands, also called the venom glands. Snakes inject this complex biochemical concoction into the target animal using specialised fangs, which, in some species, resemble hypodermic needles.
Indian subcontinent: Ground zero of snakebites
In India, over 300 species of snakes have been described to date, living in a myriad of habitats, both on land and in water. Nearly 60 species among them are thought to be capable of delivering venomous bites that are clinically significant for humans. Of these, the ‘big four’ snakes are infamous for causing the majority of venomous bites that lead to death and disability: the common cobra (Naja naja), Russell’s viper (Daboia russelii), the common krait (Bungarus caeruleus) and the saw-scaled viper (Echis carinatus).
More people suffer from snakebites in India than anywhere else in the world. In fact, more than half the global snakebite deaths occur in India. In addition to killing an estimated 46,000 people annually, Indian snakes are responsible for nearly 140,000 morbidities every year. This unsettling figure comes from a study published in 2011 in PLOS Neglected Tropical Diseases by Bijayeeni Mohapatra from the Shri Ramachandra Bhanj Medical College in Cuttack and her collaborators. The study, based on a nationwide survey, revealed, for the first time, the true burden of snakebites in India. The Indian government’s figure on snakebite fatalities in the country up until that point was less than 1,000 a year. However, the actual number of snakebite deaths and disabilities may be even higher than the estimate reported by Mohapatra’s study, as it did not cover several states in India, especially in the northeastern region. Moreover, the problem of underestimation of data is made worse because snakebite is not a notifiable disease in India.
Snakebite victims are almost always from low- and middle-income sections of the society and they tend to be the primary breadwinners of their families. Once bitten, most victims visit quacks, who resort to unscientific snakebite treatment practices. This is because people in rural India lack access to hospitals or fear not being able to afford the treatment. While the treatment of snakebites is free in government hospitals and Primary Health Centres (PHCs), its cost in private hospitals can be worth a king’s ransom. And because snakebite is a rural phenomenon, it mostly affects farmers, thus hurting the nation’s agrarian economy.
In addition to killing an estimated 46,000 people annually, Indian snakes are responsible for nearly 140,000 morbidities every year
Despite at least 200,000 Indian families being affected annually by this socio-economic malaise, the scientific and financial resources that are devoted to research on snakebites in India is shockingly low. A similar scientific neglect towards this problem in the rest of the world led the World Health Organisation (WHO) to declare snakebite as a neglected tropical disease in 2017.
Antivenom
The only scientifically validated remedy to treat snakebites is the use of antivenom. To make antivenom, venom from the target species is first collected, following which animals, such as horses and sheep, are injected with it in sublethal (incapable of killing) and subtoxic (incapable of causing harm) doses. The resulting antibodies (IgGs) produced by the animal’s immune system against venom proteins are collected, purified, and packaged in vials along with preservatives before being marketed.
The use of antivenom has saved millions of lives since it was first developed in 1895 by Albert Calmette, a French scientist at the Pasteur Institute, against the common cobra (N. naja). However, this technology has not changed since then, and there are several issues associated with how snakebites are treated even today.

Problems with antivenom
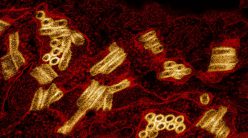
For the manufacture of commercial Indian antivenoms, animals are immunised with crude ‘whole’ venoms that contain antigens, bacteria, viruses and other impurities. In addition to toxins that could cause disease with severe symptoms in humans, snake venom cocktails also contain components that target the non-mammalian prey and predatory animals. Therefore, using crude venoms for immunisation results in the inclusion of antibodies against impurities and medically unimportant toxins, thus diluting the lifesaving antibodies in the marketed product. Studies have shown that the proportion of therapeutically relevant antibodies in an antivenom vial may be lower than 10-15 percent of the content, necessitating the use of a large number of vials for effective treatment. When excessive quantities of therapeutically redundant antivenom are administered to a snakebite victim, it can lead to further complications, including serum sickness and severe allergic reactions. But there is an even more pressing issue with antivenom, particularly in India, where the problem is already acute.
Evolution bites
Venom is thought to have evolved in the common ancestor of all snakes. This claim is supported by several lines of evidence. In fact, in a study by my colleagues and me, published in 2013 in Molecular and Cellular Proteomics, we recovered three-finger toxins (3FTx) from the saliva of an evolutionarily ancient lineage of constricting snakes, such as boas and pythons. 3FTx is amongst the most potent neurotoxic proteins that enriches the venoms of many ‘advanced’ snakes, including cobras and kraits. Thus, the discovery of these neurotoxins in ancient groups of snakes points to a single early origin of venom in this lineage.
Furthermore, as a consequence of millions of years of an evolutionary arms race with their prey and adversaries, snakes have rapidly diversified their venoms in terms of structure, function and composition. Consequently, geographically distinct populations of the same snake species can exhibit dramatic differences in venom composition, which imposes a serious problem for the production of effective antivenoms. For example, in a study on the Southern Pacific rattlesnake (Crotalus oreganus helleri), published in the Journal of Proteomics in 2014, we unravelled stark variability in the venoms of geographically close populations of this species, considered the most medically important snake in all of North America. While three of the investigated populations produced venoms rich in haemotoxins – proteins that destroy blood cells – the fourth population secreted large amounts of a potent neurotoxin – a component that targets the nervous system and causes paralysis. Since antivenom was not produced by sourcing venoms of all populations, such dramatic intrapopulation venom variation was found to severely limit its effectiveness.
As a consequence of millions of years of an evolutionary arms race with their prey and adversaries, snakes have rapidly diversified their venoms in terms of structure, function and composition
The problem with antivenom seems even more profound in India. For one, the ‘big four’ snakes – whose venoms are used to make antivenom – are not found in all regions of the Indian subcontinent. Northeast India, for example, is nearly devoid of the ‘big four’ species. This region, however, is home to many other species of medically important snakes. Similarly, while the Andaman and Nicobar Islands are politically a part of India, biogeographically speaking, they belong to Southeast Asia. Therefore, venomous snakes on these islands, such as the Andaman cobra (N. sagittifera), the Andaman krait (B. andamanensis) and the Andaman king cobra (Ophiophagous hannah), are evolutionarily more closely related to the Southeast Asian snakes than to their congeners on mainland India. But since the distribution of many of these snakes is restricted to relatively smaller geographical regions, commercial antivenoms are not manufactured against them, and clinicians administer the ‘big four’ antivenoms for treating bites from even such ‘neglected species’. It has been assumed that these antivenoms would be effective in treating bites by other venomous snakes, but this assumption has been largely untested.
The magnitude of the problem
To better understand the problem, researchers from my lab, in collaboration with our counterparts from the Gerry Martin Project and the Madras Crocodile Bank Trust and Centre for Herpetology, carried out a study that was published in 2019 in PLOS Neglected Tropical Diseases. In the study, we evaluated the effectiveness of commercial Indian antivenoms in negating the toxic effects of snakebites by the ‘neglected many’ – medically important yet neglected snake species. We compared the venom compositions, biochemical and pharmacological properties, and the potencies of the major neglected species of snakes with their ‘big four’ counterparts.
For example, we compared two populations of monocled cobra (N. kaouthia) in the eastern and northeastern part of the country (West Bengal and Arunachal Pradesh respectively) with venoms from a southwestern population (Maharashtra) of their closest ‘big four’ relative, the common cobra (N. naja). Similarly, venoms of two subspecies of saw-scaled vipers (E. c. carinatus and E. c. sochureki) and three species of kraits (B. sindanus, B. fasciatus, and B. caeruleus) from various parts of the country were examined.

Our results unravelled dramatic venom variations both between and within species. For instance, while the venom of the West Bengal population of monocled cobra was rich in neurotoxins, the venom of the Arunachal Pradesh population had more cytotoxins (toxins that destroy cells). And because of distinct feeding ecologies, differences were also observed in their venom potencies. While tests on lab mice identified the Sind krait (B. sindanus) as the most toxic snake in India (it only requires 0.37 μg of venom to kill a mouse!), and amongst the most toxic snakes in the world, the venoms of the banded krait (B. fasciatus) and Sochurek’s viper (E. c. sochureki) were found to be least potent. Such dramatic differences in potencies were explained by the differences in prey preference. The banded krait feeds voraciously on other snakes, including certain members of the ‘big four’ species, while the preferred prey for Sochurek’s vipers are scorpions. Hence, the venoms of these snakes may be highly potent against their non-mammalian prey, but they were found to be less potent against mammals.
Our study revealed alarming shortcomings in contemporary snakebite therapy in India
Finally, our study revealed alarming shortcomings in contemporary snakebite therapy in India, as the antivenoms not only failed to counter the toxic effects of many neglected species, but also failed against the North Indian population of the common krait, a ‘big four’ snake. Ongoing research in our lab is unravelling astonishing variations in venoms, even within the same populations, and extremely disturbing deficiencies of the conventional antivenom in treating bites from the geographically disparate populations of the ‘big four’ snakes.
The way forward
Unfortunately, nearly all antivenom manufacturers in India produce antivenoms by sourcing venoms from just one part of the country. These venoms are collected by the Irula Snake Catchers Industrial Cooperative Society from mostly two districts in Tamil Nadu – Kanchipuram and Thiruvallur. In the face of this spectacular geographic venom variability, how can we ever address the snakebite crisis in India?
The solution may lie in new approaches and cutting-edge technologies being adopted by toxinologists and venom biologists from around the world – from producing venoms in plates with the help of venom organoids (organs grown on plates) to the mass production of antivenoms in cell cultures. One such unconventional approach is being pursued by our lab. Using our understanding of venoms, we are seeking to produce broadly neutralising antivenoms – antidotes that are effective against geographically distinct populations and/or species of snakes. Our pursuit to innovate Next Generation Antivenoms (NGA), amongst other strategies, involves the discovery of antibodies against the evolutionarily conserved regions in toxin proteins that are shared between distinct populations and species across India. Broadly neutralising antivenoms generated this way will be inexpensive, dose efficacious, and effective in treating snakebites across the country. Unfortunately, India needs to wait a bit longer for its NGA as such recombinant antivenoms will require human clinical trials.
Kartik Sunagar is an assistant professor at the Centre for Ecological Sciences where he leads the Evolutionary Venomics lab