Digital technologies are changing research and treatment
(Photo: Parul Yadav)
In 2018, Vijay Chandru was already thinking about pandemics.
He was back on the IISc campus, where he had co-founded India’s earliest genomics startup, Strand Life Sciences, nearly 20 years ago. Now a visiting faculty member at the Department of Bioengineering (BE), he started teaching a course on digital epidemiology, using mathematical models to walk students through “nightmare scenarios” in which an infectious disease spreads quickly among large populations. “I showed them a live simulation of a COVID-like pandemic,” he recalls.
Two years later, Vijay watched as the same scenarios eerily began to play out in real life.
COVID-19 was devastating. But it also created the “perfect storm” for the rise of digital technologies, Vijay says. Hospitals offered online consultations. Scientists used machine learning models to scan X-ray images for signs of COVID-19. Digital databases of infections and vaccinations greatly helped policymakers. “Suddenly, many things were happening,” says Vijay.
The idea of ‘digital healthcare’ has been around for a while. For decades, clinicians have been using computers to record and analyse patients’ health data. Today, doctors use WhatsApp and Zoom to talk to patients in remote areas. Some of us use smartwatches to track our pulse rate and blood pressure.
It’s not just the pandemic that has prompted this shift. The medical profession is grappling with several crises, writes former physician and journalist James le Fanu in his book, The Rise and Fall of Modern Medicine. More and more doctors are becoming “bored and disillusioned”. Many people are becoming obsessed with “trivial or non-existent” threats to their health. Alternative therapies – mostly unregulated and untested – are soaring in popularity. And hospital visits are becoming too expensive.
The medical profession is grappling with several crises
In India, there are additional problems: Awareness about health and disease is poor in rural areas, urban areas have better access and good hospitals but at a high cost, and the country’s population far exceeds the number of healthcare professionals.
Perhaps digital technologies could address some of these issues, writes GK Ananthasuresh, Professor at the Department of Mechanical Engineering, in the editorial for the Journal of the Indian Institute of Science’s 2020 issue on digital health.
Ananthasuresh is one of several faculty members at the Institute leading efforts to build an ‘IISc digital health initiative’. “The idea came from Vijay Chandru,” he recalls. “He wanted to see if IISc could set up a digital hospital.”
The motivation is to explore possibilities beyond telemedicine and electronic health records. Several projects have been started under this umbrella – developing AI models for diagnosis, tracking blood biomarkers before the onset of disease, building digital replicas of organs, and even creating artificial organ systems in the lab. Some projects are aimed at finding better ways to treat and manage specific diseases, like diabetes. “When we use digital technologies in healthcare,” Ananthasuresh says, “there is no end.”
AI in the ICU
In 1949, German physician Wolf-Dieter Keidel beamed a low-frequency sound wave into a patient’s chest to obtain an ‘acoustic heart shadow’ – the earliest attempt at echocardiography, now used widely by sonographers and doctors to find abnormalities in the heart. But today’s outpatient departments (OPDs) and Intensive Care Units (ICUs) are so crowded that they simply don’t have the time to do a proper echocardiogram or analyse it closely, says Farhan Adam Mukadam, PhD student at BE, who completed his MD at CMC Vellore.
“Every morning, for every patient, a doctor has to look at around 250 data points,” he says. “If something is churning this data and giving insight, it can change performance in the ICU and save lives.”
That “something” in recent years has been machine learning (ML) models, which can continuously scan images and videos of a patient’s beating heart to spot abnormalities. Farhan has been working with KVS Hari, Professor at the Department of Electrical Communication Engineering, to train such models – called neural networks – using anonymised patients’ data from the Sri Jayadeva Institute of Cardiovascular Science and Research.
ML models can continuously scan images and videos of a patient’s beating heart to spot abnormalities
The goal is to get the models to give as accurate a report as a sonographer would. For example, the left ventricular ejection fraction (LVEF) – the quantity of blood pumped with each heartbeat – is usually calculated by the sonographer after looking at an echocardiograph. A value below a certain percentage indicates a poorly performing heart. However, the sonographer has to measure the value repeatedly and accurately, especially to track subtle changes. Such a repetitive task can be done by an ML model. “It’s a five-second job for the model,” says Farhan.
But the problem, he explains, is that the large amounts of clearly labelled datasets – images and videos – needed to accurately train these models are lacking in India, and even the ones available abroad are limited to a single “view” of the heart. “There is no comprehensive echocardiography dataset globally,” Farhan adds. “If we create our own datasets, we will be able to answer clinical questions both for stable patients in the OPD and unstable patients in the ICU.” So far, he has collected and labelled data from close to 6,300 patients – more than half of the roughly 10,000 datasets that would be ideal for training the models.
Eventually, such models might also help predict the risk of developing a disease, like diabetes.
“A few years ago, a really cool study from Israel used machine learning to predict which pregnant women could develop gestational diabetes based on their past health records,” explains Siddharth Jhunjhunwala, Associate Professor at BE.
But in India, such past health records don’t exist. “These exist in the UK, Israel and the USA, because everybody comes for regular health checkups. For the same individual, one can collect data as they age, to track disease progression,” he explains. “[In India], ICMR does cross-sectional data collection … from maybe 2-3 lakh people, at a given time. But they might not go back to the same individual again.”
To address this problem, Siddharth’s lab has started a pilot study through the IISc Health Centre to collect blood samples from a few hundred middle-aged individuals. The plan is to record about 30 different health risk factors apart from just blood glucose – serum creatinine, lipids, cholesterol, thyroid stimulating hormone and more – every six months, over many years. “If I have all this data available, then maybe by looking at a combination, say, a blood glucose level of 100, plus a cholesterol level that’s higher, plus an hBA1C level that’s borderline … we could successfully predict the onset of diabetes and its progression.”
Siddharth’s team also plans to make the data available in a public repository so that other researchers can use it for building ML models, or for more advanced applications like digital twins.
Carbon copy
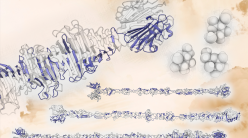
When Strand Life Sciences was founded in 2000, the idea of digital twins – computer simulations that recreate entire machine parts and processes – was gathering steam. The fledgling startup was interested in something quite ambitious: Building a digital twin of a human organ, the liver.
The project was spearheaded by one of their newest recruits, Kalyanasundaram Subramanian, who was concerned that many drug trials failed because researchers couldn’t predict how the drug molecule could harm the liver. At that time, many people were focusing on the drug properties alone, and trying to get their models to predict whether a certain property would cause cell death or other harmful effects.
“We had to take a different approach,” Vijay says. The Strand team used hundreds of differential equations to recreate a computer simulation of a liver in homeostasis (stable condition), track how a drug molecule would disrupt this state, and whether the liver could return to its original condition.
The Strand team used hundreds of differential equations to recreate a computer simulation of a liver in homeostasis
Another challenge was that every drug molecule gets broken down into many smaller components, called metabolites. “It was very difficult to simulate how these metabolites are generated,” Vijay explains. The team then decided to combine their simulation with a lab setup in which drug metabolism was tracked in live liver cells. The combination snagged them a “strong” patent in the USA, and several requests from drug companies willing to pay them USD 10,000 per head to evaluate their drug candidates. “It was a completely new idea,” Vijay recalls. In 2016, 12 years after they had started the project, Syngene International, the services arm of the company Biocon, bought out their digital liver technology.
More recently, Ananthasuresh’s team has been working on building a digital twin of the foot, to understand how foot ulcers and other harmful complications can be mitigated in people with diabetes. “There’s a dangerous disease called Charcot’s foot in diabetic patients where the bones will collapse and fuse together. They may not even feel pain,” he explains. “After a point, it becomes irreversible, and then [the only solution] is amputation.”
His team constructed a computer model of the foot and tested how accurately it could estimate plantar pressure (the pressure felt by our soles when we walk), with or without insoles. This helped them develop a special set of customisable insoles in collaboration with the Karnataka Institute of Endocrinology and Research (KIER), with support from the Rajiv Gandhi University of Health Sciences. The insoles use simple snapping arches to dynamically offload high-pressure regions while walking, to avoid ulcer formation.
Ananthasuresh is also working with KIER to build “digital foot kiosks” that can be installed in urban areas like malls and in rural post offices and primary health centres, where triaging can be done. A person simply has to place their foot on the device and by measuring their plantar pressure, temperature and other factors, the machine could spit out a report on their foot health and inform them if they are at risk of developing ulcers or other complications. Such interventions are direly needed in India, especially in rural areas where people might not even be aware that they have diabetes, Ananthasuresh says.
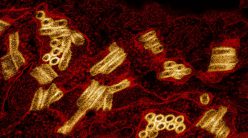
In recent years, the idea of building replicas that combine both the physical and the digital, called ‘organ-on-a-chip’, is also becoming popular, driven not just by the spiralling cost of drug development but also ethical concerns about the use of animal models. Scientists are building 3D platforms in the lab out of soft materials and gel matrices in which tissues are able to grow and divide just like how they would inside the body, explains Kaushik Chatterjee, Professor at the Department of Materials Engineering. His team is currently working on building a lung-on-a-chip, in collaboration with the lab of Deepak Saini, Professor in the Department of Developmental Biology and Genetics.
Building replicas that combine both the physical and the digital, called ‘organ-on-a-chip’, is becoming popular
“You can mould materials into nanochannels, and start flowing liquid through the channels. In the case of lungs, you also need something that expands and contracts. So if you have an artificial membrane – with air flowing on one side, and blood on the other – where gaseous exchange can happen, you are really starting to talk about a lung mimic,” he explains. Such systems can be integrated with digital data feeds and tools to test the effects of different drugs and therapies.
When the prototype is in place, Kaushik’s team plans to use it to study the harmful effects of both pollutants and infectious viruses. They are specifically focusing on a condition called fibrosis, where the lungs become stiff and cause breathing difficulties.
Once they are able to build such organ replicas, the next step would be to try and integrate multiple organs on chips, Kaushik adds. “Say you have a little matrix where you have cancer cells growing in tumour masses. What if, after a cancer drug has passed through this ‘tumour chip’, it could flow into a ‘liver chip’ to see whether the liver is getting damaged or not, and then maybe flow into a ‘heart chip’ to see whether it is causing cardiotoxicity? Now, if you start integrating a number of such ‘tissues’ together, you can have a ‘body-on-a-chip’. Then we can study not just the effect [of the drug] on individual organs. We can, in principle, recreate the whole human physiology.”
Time for reform
Back in January 2021, at the height of the pandemic, Vijay was invited to join the Lancet Citizens’ Commission, a panel formed to analyse gaps in India’s healthcare systems and provide a roadmap to achieve universal healthcare by 2030. “It was a response to how ill-prepared we were for the pandemic,” explains Vijay. One of the first things the commission did was carry out surveys among citizens and healthcare workers. “A majority of the citizens are actually saying that they want technology [in healthcare],” Vijay adds.
Vijay feels that the digital healthcare revolution can also happen at the community level. Two years ago, for example, to track the health of pregnant women in rural Karnataka, the Public Health Foundation of India armed ASHAs (Accredited Social Health Activists) with a multilingual software tool called M-CAT. This tool greatly helped them record door-to-door data more efficiently and also quickly diagnose some common health risks.
Vijay believes that the advent of digital technologies has given the country a chance to revamp its health systems. “Digital health has now become a central topic in healthcare reform,” he says. In 2021, the Government of India launched a National Digital Health Mission; among other goals, it aims to create long-term electronic health datasets and introduce more digital services in healthcare, like standardised health IDs – similar to Aadhar – for each citizen.
Digital healthcare initiatives are also receiving a boost from philanthropists who are supporting new centres at institutes like IIT Bombay, Ashoka University and IISc, Vijay points out. “With the hospital coming up here on campus, I think IISc has a fantastic opportunity to drive the agenda for digital health in the country.”