A former IISc student, now an educator, remembers her experience of navigating issues with mental wellness and lays down what she learned from it
She walks alongside her mentor,
enters the seminar hall and gets comfy in her seat.
She is sinking through the seat,
a black hole sucking her in,
her vision blurs, and she’s falling
She’s falling
The speaker’s words are distant murmurs,
as if in a dream,
her own words unreachable,
masking a muffled scream.
Sometime in late September 2021, when I decided to write this piece on mental wellness on campus, I was immediately transported back to a mid-September 2012 afternoon – my second month in IISc – that was about to change the very trajectory of my academic career. It was my first and pretty dramatic glimpse into what a mental health struggle could look like. But more than that, it was the experience that followed that opened my eyes to the factors creating a dearth of mental wellness in academia.
Speak to any grad student, and they would have several stories to share about labs where supervisors expect students to prioritise experiments over meals, or work on weekends and holidays even when their projects don’t demand it. I have known peers who expressed the need to hide their engagement in non-academic activities after work hours, friends who have worried about taking time off to visit family or friends. I remember that in my first year of the Integrated PhD programme, most of our course assessments were scheduled at odd hours on non-working days, leaving little room for recreational activity. It was not rare, even in those very early days of my doctoral years, to encounter peers judging their labmates on the hours they spent in lab, on whether they were “dedicated” and “passionate” enough to spend their weekends in the lab, indicating that this unhealthy and unprofessional work culture has been pervading generations of researchers.
However, the culture of poor to non-existent work-life balance is not limited to a PhD scholar’s experience, or even academia. Superhuman expectations of “productivity” affect every member of an organisation or institution, where adjectives like “resilient”, “high-functional despite”, “productive despite” turn into sought-after labels that insidiously exclude the workplace accommodations required by those whose mental wellness conditions call for a long-term supportive and inclusive environment. It doesn’t help that mentors and supervisors often shy away from opening up about their own struggles or the workplace accommodations they might have appreciated in this regard. Their reticence leaves little room for mentees and students to gain confidence or to feel safe about opening up in their workplace. The role models held up to us are always the ones who overcome struggles with little to no help from others, grinding their teeth and ‘battling it through with sheer grit’, ‘always thinking about their research’. I think many of us invariably attempt to ape these qualities, and any failure or departure from these models triggers a crisis of self-esteem and self-doubt, eventually creating a vicious cycle that is difficult to break away from.
What we need is room for open and transparent conversations about mental health amongst all stakeholders interacting in a system – students, faculty and staff
Furthermore, our tendency to promote only the professional success stories of those who overcame their struggles with mental health creates the misconception that it is a one-time hurdle needing a one-time resolution. I agree that success stories can be the bearers of hope to someone who’s unable to see the light at the end of the tunnel, but at the same time, it can feel alienating to those for whom the struggle doesn’t end with tackling that one-time hurdle. The nature of support these individuals need might look quite different from those for whom the concerns were limited to a specific time, place or environment. What we need is room for open and transparent conversations about mental health amongst all stakeholders interacting in a system – students, faculty and staff. Of course, the choice of sharing lies with the individual – it is the fear that stops them from sharing that is worrisome. The stigma around mental health is strong enough that I have seen people admitting to having problems fearing that they will be perceived as “unreliable”, “less productive” and “irresponsible”. This creates a communication gap, not only for those seeking support at their workplace but even for those who want to help someone who might be struggling, but there is no frame of reference to turn to in either case.
Empathetic language to ask a person what help they need would go a long way towards bridging this gap. Such empathetic and inclusive language might come naturally to some, while some of us may need to be trained in this skill (building empathy in a community is already being practiced in institutes across the world, particularly in schools, which can act as a source of inspiration for academia). Without it, we risk imposing improper remedies on others without consulting them. Even if well intentioned, these actions can aggravate a mental health problem that we may not have adequate insight on. For example, the preconceived notion that being with family would aid recovery can lead to students who are unwell being sent home against their wishes. This not only violates their autonomy as adults, but can be particularly traumatising for individuals hailing from dysfunctional families and whose mental health struggles are deeply rooted in their personal history.
The official conversations on mental health on campus have mostly focused on the concerns of individuals with mental health conditions like depression and anxiety, and prevention of suicide. But what about the overlooked section of people who are reeling from chronic stress, or cornered in a non-inclusive workspace, yet are not quite in a place where they can be diagnosed with any serious mental health condition? I remember being told by a health professional, “Everyone has mild to moderate depression, why should that necessitate time off from work or a change of work environment for recovery?” Does that imply there is no place for those lacking mental wellness unless it escalates to a mental illness?
I have come across numerous instances of mental health professionals dismissing my friends’ concerns about their health, or worse, jumping to conclusions and diagnoses too soon, or prescribing medications a little too hastily – sometimes, inappropriately without proper diagnosis – which from my experience can sometimes worsen the mental health condition. Besides, for me and many of my peers, the task of finding a “compatible” mental health professional and getting a proper diagnosis through trial and error has been an excruciatingly long and exhausting task. This in no way suggests that all mental health professionals are judgemental or dismissive, nor does it imply that medication and therapy is futile. I have personally interacted with several who are particularly empathetic, have exceptionally inclusive perspectives and who are also aware of these loopholes in the field, and work relentlessly to improve the situation.
Is there no place for those lacking mental wellness unless it escalates to a mental illness?
While mental health professionals may rightly advocate for a healthy lifestyle, rarely is the feasibility of this healthy lifestyle examined from the perspective of a student living on a meagre stipend and trying to keep up with a work schedule that demands, lauds, and often rewards overwork. Poor work-life balance can adversely affect both physical and mental health, as is experienced in burnout. This makes me wonder whether an individual can actually be helped in the long term in such an environment solely by turning to a mental health professional.
Where the lack of mental wellness is being triggered or worsened on a systemic level, to place the onus of one’s own mental health entirely on the individual can never be quite sustainable, if at all successful, when the environment plays such a key role in not only one’s mental wellness but overall well-being. Does it mean one should never aim for great outputs, ambitious goals? Of course, one should! It is not the destination that needs switching always, but the road to the goals that needs to be better paved instead of expecting every following generation to wade through murky waters and wince through the dingy and bumpy alleys that we, the predecessors, have gotten so used to. Changing this might require an enormous amount of creativity and empathy, and organised effort, but unless a determined initiative is taken, the path will remain ridden with potholes for generations to come.
In some ways, the rise in mental unwellness with the pandemic, a multidimensional stressor, has revealed these gaping holes in our conversations around mental health and mental healthcare. And it has directed us to the changes that are required in our approach to address these issues. For instance, while everyone to some extent has suffered the brunt of this immense stressor, I did notice that those who recovered fairly quickly or easily from the blows were not simply resilient individuals, they were often the ones in a more resilient environment, cushioned with a reliable and inclusive support system, with easy access to proper and affordable healthcare, a steady income, and a relatively stable and healthy professional and personal life. The workplace might not be able to do much to change the personal past and present of an individual, but creating an inclusive environment that provides stability in at least one facet of one’s life can sometimes be the anchor that one needs to sail through the changing tides of life. As simple a thing as timely disbursement of a stipend could mean one less major stressor in a researcher’s already uncertain life, without the additional stress of losing out on the time and energy it takes to follow up with the relevant office.
Ensuring an environment that fosters mental wellness is key to keeping mental illness at bay. In the institute I currently work in as an educator, the institute counsellor, mentors, teachers and the institute authority often work hand in hand with the students, without breaching confidentiality, to understand each student’s requirements, creating an inclusive environment that prioritises trust and safety. This eventually sets the students up for growth and long-term success, even if it were to mean a temporary setback in terms of deadlines.
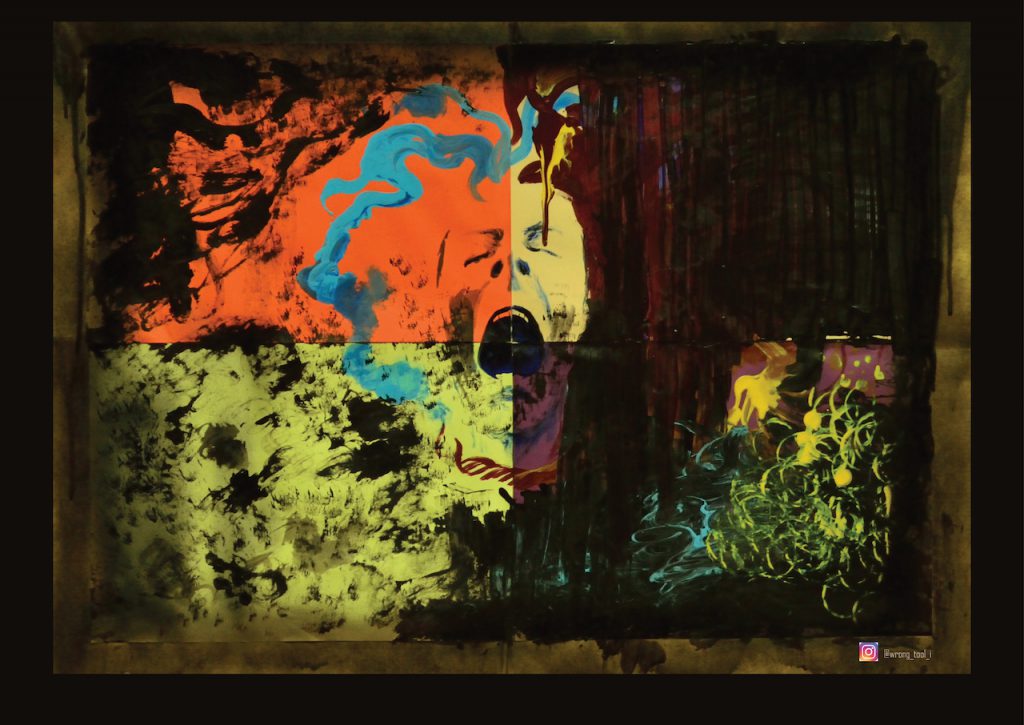
Lastly, I think the answer to our collective burnout is probably not just sessions with a therapist, but as one of my friends recently suggested: “the answer lies in a life offering sustainable rewards”. For me, sustainable rewards in life range from accessing the flow state of mind during art sessions with friends or on my own, or playing with data (for fun), to just taking a break to embrace the stillness and soak in nature, doing nothing conventionally “productive”. It might be something entirely different for another person. It would be wonderful to have an environment where all members of the institute have access to these moments or sometimes, even periods to unwind, to create space for these rewards in an otherwise deadline-driven “always busy” work life. For in the end, I know that no number of therapy sessions could have replaced the amazing support system I was lucky enough to have landed during my PhD, despite all odds and despite all their shortcomings, in the form of an understanding mentor, life-long friends, the thrill of learning new skills, indulging in creative expression, and last but not the least, countless walks through the green campus of IISc.
Sambita Modak is a former PhD student at the Centre for Ecological Sciences, IISc, and was also a member of Empaths at IISc. She is currently working as an educator at Bombay International School and is interested in psychology, art, and the need for systemic change to foster a more inclusive and healthy workplace environment.




