Learning what activates cancer stem cells, which can lead to metastasis, may hold the key to fighting other cancers too

Annapoorni Rangarajan, Associate Professor at the Centre for Molecular Reproduction and Developmental Genetics, was bitten by what she calls the “cancer keeda” over two decades ago as a Master’s student at Nagpur University. “What really interested me was how a normal cell in our body could convert to a cancer cell,” she says. “It’s not so altered that the body’s immune system rejects it. At the same time, it’s different, and it’s out of control. So what goes wrong?”
In 2004, armed with a PhD from the National Centre for Biological Sciences and having just completed her postdoc at the Whitehead Institute for Biomedical Research in the US, she moved to IISc at a significant time: oral and cervical cancers were the highest-occurring ones in India, but in cities, breast cancer posed a large problem, threatening to overtake cervical cancer (it is now the leading cause of cancer deaths among Indian women).
Rangarajan moved to IISc in 2004, a significant time for the epidemiology of cancer in India: oral and cervical cancers were the highest-occurring ones in India, but in cities, breast cancer posed a large problem
It was also an important period in terms of how cancer biologists had begun to understand the disease: in 2003, scientists at the University of Michigan Comprehensive Cancer Centre identified breast cancer stem cells for the first time, and the fields of stem cell research and cancer research were starting to overlap. A tiny subpopulation of cells, among normal cells as well as cancer cells, were found to show stem cell-like properties (namely, the ability to develop into different cell types and divide to produce more stem cells), and were able to live and grow even after detaching from the substratum.
In an ordinary cell, this detachment leads to cell death. It is hypothesised that cancer stem cells, however, are able to survive in suspension and travel through blood vessels to a different part of the body to form a new tumour. Such spreading of cancer in the body – known as metastasis – is responsible for an overwhelmingly large number of cancer deaths, and that was where Rangarajan’s focus on cancer research came in.
Spreading of cancer in the body – known as metastasis – is responsible for an overwhelmingly large number of cancer deaths, and that was where Rangarajan’s focus on cancer research came in
“My [question] when I started my lab at IISc was, can I isolate these cancer stem cells, and learn the molecular mechanisms for how they grow in an anchorage-independent fashion?” she says. “It is the only kind of cell that can re-create a tumour, and is also, to an extent, drug-resistant as it survives chemotherapy. Fundamentally, can I understand the stem-like properties in them? And therapeutically, can I find out new mechanisms through which we can target them?”
When Rangarajan started out as an independent researcher, she says, “I did not want to deal with cell lines, which is what every biology lab was doing at the time.” (If we know of cancer cell lines in popular culture today, perhaps it’s because of the infamous HeLa cell line, named after Henrietta Lacks, whose cancer cells were taken in 1951 and cultured without her knowledge or consent – now the subject of a recent movie starring Oprah Winfrey.) Instead, Rangarajan collaborated with the Kidwai Memorial Institute of Oncology in Bengaluru to obtain breast tissue biopsies and isolate the cancer cells for further study.

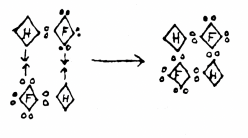
As a tumour grows, its Trojan Horse-like stem cells go into a hibernation of sorts, cutting down on nutrients and energy use to save them for later. Stresses that lead to depletion of energy activate a protein within cells called AMP-activated protein kinase or AMPK. The first “eureka moment” in her laboratory, says Rangarajan, was when they identified matrix detachment as a form of stress that super-activates AMPK. The second such moment was establishing that inhibiting AMPK prevented the growth of mammospheres, or clumps of breast cancer cells. Recent work in her lab reveals that once it is activated by stress, AMPK combines the “axis of evil” in terms of drug resistance: it makes the cells more drug resistant in suspension, transforms its shape to penetrate and exit blood vessels, and enhances its stem cell-like qualities so that it travels through the body until it latches onto a new organ and forms another tumour.
The first “eureka moment” in her laboratory, says Rangarajan, was when they identified matrix detachment as a form of stress that super-activates AMPK
In 2015, in an innovative step taken with Kaushik Chatterjee, Associate Professor at the Materials Research Centre, porous 3D scaffolds were created on which they could grow breast cancer cells that mimicked tumour growth in humans far better than the existing 2D plates, and was cheaper than using animal models. Currently, they are developing patient-specific 3D models of tumours which they plan to use for drug screening.
Targeting AMPK seemed to hold the key to achieving this. While chemotherapy kills the bulk of cancer cells, it actually appears to enrich cancer stem cells, which can cause a relapse later on, Rangarajan says. “In the absence of AMPK, commonly used chemotherapeutic drugs like doxorubicin can target and kill cells far better. Inhibition of AMPK, in combination with existing chemotherapeutic drugs, is probably an effective option.” Currently, her team is collaborating with HS Atreya, Professor at the NMR Research Centre, to make peptide inhibitors for AMPK. “It will be a good 10 years before it enters the market,” she says.
“Inhibition of AMPK, in combination with existing chemotherapeutic drugs, is probably an effective option.”
Rangarajan’s work on the role of AMPK in breast cancer is especially significant as AMPK plays a role in other epithelial cancers; learning how to inhibit AMPK could mean advances in treatment for other kinds of cancer as well.
Currently, Rangarajan is studying the link AMPK might provide between diabetes and breast cancer. A widely used anti-diabetic drug, metformin, is also used to treat cancer, but activates AMPK in the bargain. “What if you treat a patient for diabetes but place them at a higher risk of developing cancer that spreads? And if you have a patient who’s got both, what kind of treatment and strategies should we predict for them?” They’re big questions, with important implications for healthcare in India and the world. “They’re in our next Five Year Plan,” she jokes.